Medical therapy
Medical therapy refers to the use of prescription medication to treat specific risk factors or medical illnesses. There are a wide range of proven and effective drug therapies in the field of cardiovascular medicine aimed at alleviating symptoms, slowing progression of disease and improving survival.
| Blood thinners (anti-platelets/ anticoagulants) |
Cholesterol | Blood Pressure | Angina | Arrhythmia | Heart Failure |
|---|---|---|---|---|---|
| Aspirin | Statins | Angiotensin converting enzyme inhibitors (ACEi) |
Beta-blockers | Beta-blockers | Loop diuretics |
| Clopidogrel | Fibrates | Angiotensin II receptor blockers (ARB) |
Calcium channel antagonists | Calcium channel antagonists | Angiotensin converting enzyme inhibitors (ACEi) |
| Ticagrelor | Calcium channel antagonists | Nitrates | Digoxin | Angiotensin II receptor blockers (ARB) |
|
| Prasugrel | Thiazide diuretics | Nicorandil | Flecainide | Beta-blockers | |
| Warfarin | Alpha-blockers | Ranolazine | Sotolol | Eplerenone | |
| DOAC | Spironolactone | Amiodarone | Spironolactone | ||
| Beta-blockers | Sacubitril/Valsartan |
A cardiology specialist would assess your symptoms and risk factors carefully before considering appropriate cardiovascular investigation. This evaluation could confirm a specific diagnosis which may be helped by medical therapy. We can advise you as to the best available treatment options, potential side effects and monitoring requirements.
Coronary angioplasty (PCI)
Invasive coronary angiography may confirm significant narrowing, or stenosis, of one or more areas in the coronary arteries which may benefit from coronary angioplasty with stent insertion, or sometimes referred to percutaneous coronary intervention (PCI).

Pre PCI

Post PCI
Coronary angioplasty involves the direct treatment of a narrowing or blockage of the coronary arteries to improve angina or treat a heart attack in an emergency setting. The procedure is performed after coronary angiography, under local anaesthetic with direct X-ray guidance and intravenous contrast dye. Initially, a guide catheter is passed up to the coronary artery in question, using either the radial artery in the wrist or femoral artery at the top of the leg. A thin metal wire is then passed across the culprit arterial narrowing to allow the use of a small balloon to stretch, and coronary stent placement to keep, the blood vessel open in order to improve circulation.
The patient usually spends one night in hospital and requires the strict use of long term dual blood thinner medication, such as Aspirin and Clopidogrel, statin therapy and anti-anginal medical therapy. There are small procedural risks to consider including heart attack, stroke and bleeding, which would be discussed in detail by your cardiac specialist.
Permanent Pacemaker (PPM) insertion
A conventional permanent pacemaker (PPM) is a small device containing a battery and automatic generator connected to one or two electrical leads. This invasive procedure is used to treat slow abnormal heart rhythms, known as bradyarrhythmia.
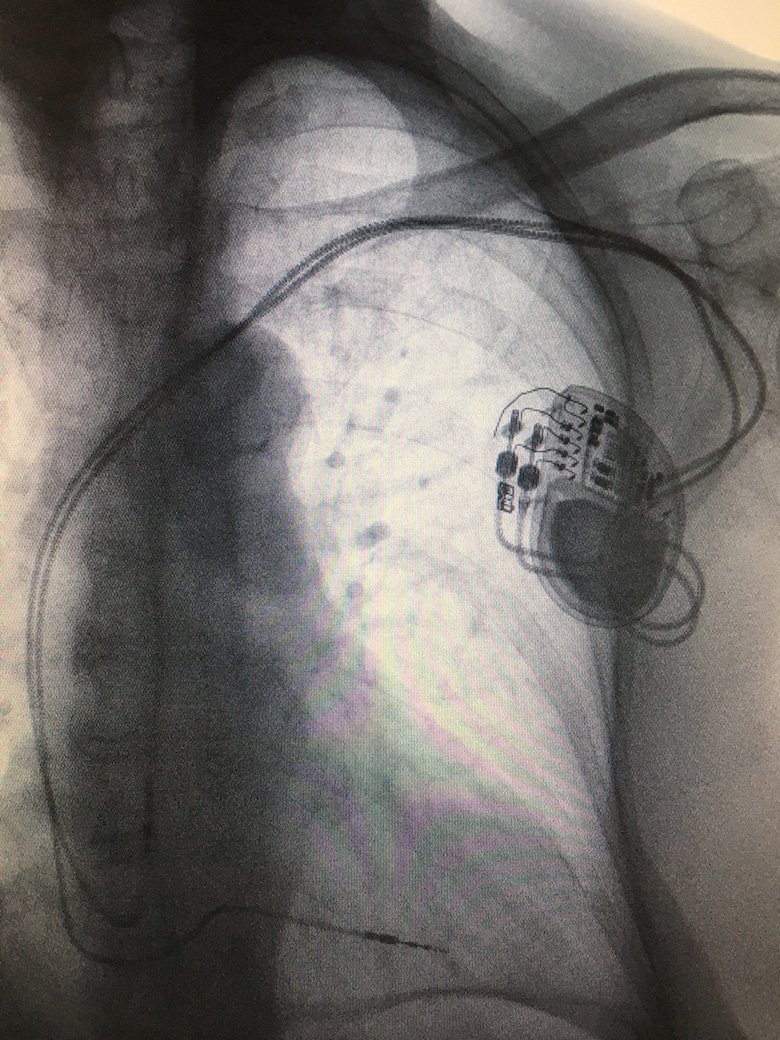
Dual chamber pacemaker
The procedure is performed by a cardiologist, under local anaesthetic and light sedation, in sterile surgical conditions. A 3-4cm incision is made on the chest wall approximately 1cm below the collar bone. The subclavian, axillary or cephalic veins are located close to here. These are accessed to pass and secure electrical leads under X-ray guidance, within the right ventricle and right atrium, if required, before connecting to a pacemaker device.
After the pacemaker is fitted, patients usually stay overnight in hospital and undergo a chest X-ray, pacemaker check and wound review before being discharged home. Heart rhythm pacing devices require regular long term follow up after discharge. Conventional pacemaker battery life can last 8-10 years, depending on individual use and circumstances, before requiring a battery change procedure.
Pacemaker procedures are invasive and involve permanent implants. There are small degrees of risks involved, including infection, bleeding, lead displacement, pneumothorax (puncture of the lung), tamponade (puncture of the heart) and lead failure, which would be discussed in advance with your specialist.
Implantable Cardioverter-Defibrillator (ICD) and cardiac resynchronisation therapy (CRT)
Patients with a known history of cardiac arrest and ventricular tachyarrhythmia, or if considered at high risk of such events, may be offered an Implantable Cardioverter-Defibrillator (ICD). An ICD device is larger than a conventional pacemaker and can be connected to an electrical defibrillator-pacing lead and, if required, a standard atrial pacemaker lead.
Selected patients with symptomatic heart failure may benefit from an additional left ventricular pacemaker lead positioned within the coronary sinus vein. This is known as cardiac resynchronisation therapy (CRT), which can improve heart function, symptoms and prognosis. CRT can be combined with an ICD, known as CRTD, or simply as a pacemaker, or CRTP.
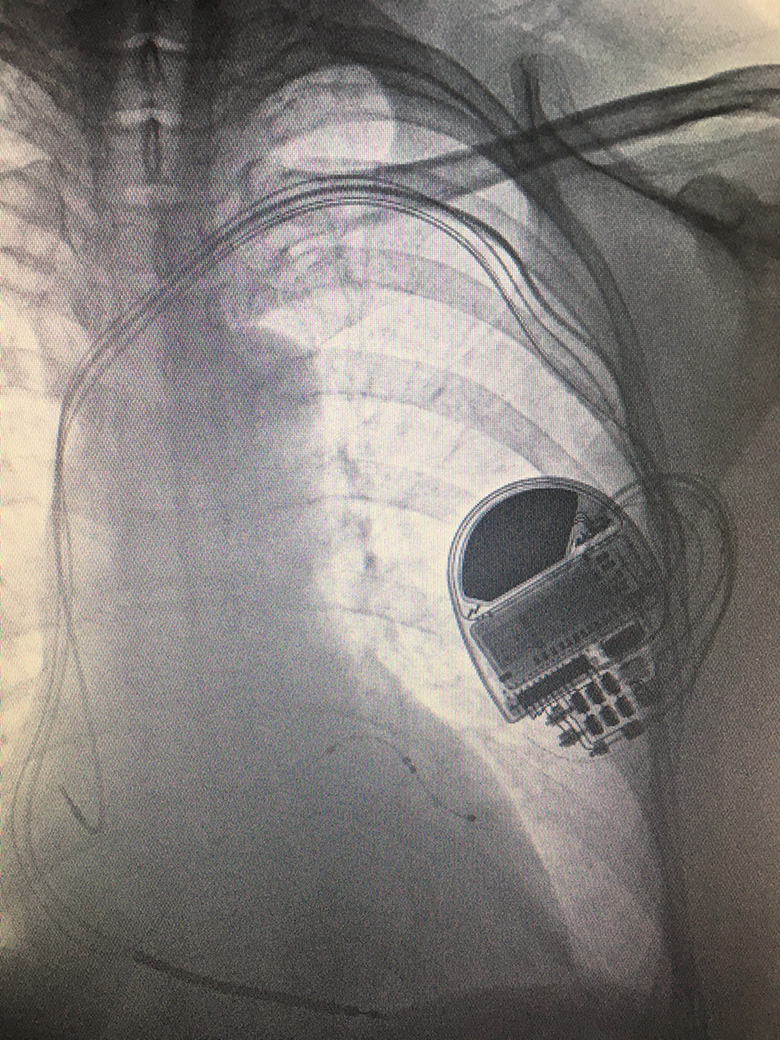
Biventricular ICD (CRTD)
The procedure is performed by a cardiologist, under local anaesthetic and light sedation, in sterile surgical conditions. A 4-5cm incision is made on the chest wall approximately 1cm below the collar bone. The subclavian, axillary or cephalic veins located here are accessed, in the same way as a pacemaker procedure, to position electrical leads within the right ventricle, right atrium and coronary sinus vein, as required, under X-ray guidance before connecting to a ICD/CRT device.
After the device is fitted, patients usually stay overnight in hospital and undergo a chest X-ray, device check and wound review before being discharged home. Heart rhythm devices require regular long term follow up after discharge. ICD/CRT device battery life can last up to 6 years, depending on individual use and circumstances, before requiring a battery change procedure.
ICD/CRT device insertion procedures are invasive and involve permanent implants. There are small degrees of risks involved, including infection, bleeding, lead displacement, pneumothorax (puncture of the lung), tamponade (puncture of the heart), lead failure and inappropriate shocks, which would be discussed further with your specialist.
Catheter ablation
Catheter ablation is an invasive procedure performed to treat symptoms caused by various forms of arrhythmia, including atrial fibrillation, atrial flutter, SVT and accessory pathways, which have not been controlled by medical therapy or where the latter has not been tolerated due to side effects.
The procedure is carried out under sedation or general anaesthesia. It initially involves passing thin catheters, inserted in the femoral vein at the top of the leg, to access the right atrium of the heart under X-ray guidance. An electrophysiological study is performed to identify the origin of the arrhythmia.
In some patients, depending on the cause of the arrhythmia, the ablation will take place on the right side of the heart. Certain patients may require access to the left atrium and pulmonary veins such as treating atrial fibrillation. In this scenario, a transoesophageal echocardiogram may be required to exclude clots and aid crossing the interatrial septum. Radiofrequency energy is then transmitted to specific targets identified within the heart. This creates heat which destroys the affected area and aims to block abnormal electrical activity to treat the underlying condition.
This is an invasive procedure that carries a small degree of risk, including stroke, tamponade (puncture of the heart), femoral blood vessel damage, nerve damage, atrio-oesophageal fistula or need for pacemaker insertion. The risks and benefits would be discuss with you in detail by your cardiac specialist.
Cardiac surgery and TAVI
Cardiac surgery is considered if you have severe valvular heart disease and/or severe multi-vessel coronary artery disease. These are major open heart operations performed routinely under general anaesthetic. Patients should expect to stay in hospital for one week, if there are no complications, and expect a minimum recovery period of 6-10 weeks.
A detailed pre-operative assessment is required to assess suitability for surgery including blood tests, echocardiography, 12-lead ECG, coronary angiography, lung function testing and carotid artery scanning. It is important to determine the type, complexity and risk of operation and establish that potential benefit outweighs risks. It is also important to have a discussion with regards the choices available to you, such as the most suitable type of heart valve replacement.
Certain high-risk patients with severe aortic stenosis, not amenable to conventional surgery, may be suitable for a less invasive Transcatheter Aortic Valve Intervention procedure, known as TAVI. In this procedure, a replacement valve is generally passed via the femoral artery (trans-femoral) or directly (trans-apical) and positioned in the heart.

